There is a steadily increasing need for temperature management.
Globally, 234 million major surgeries occur each year where the use of a temperature probe is recommended.1,2
Guidelines require monitoring of patient temperature during anesthetic procedures where a change in body temperature are intended, anticipated, or suspected.2,3
In the US alone, it is estimated that greater than 54 million procedures require the use of a temperature probe every year3
Patients in surgery are at risk when their temperature fluctuates.
Hypothermia
Hypothermia is extremely common during surgery, but can also be life-threatening. Hypothermia can cause increased oxygen consumption, increased cardiac output, shivering and pain, increase in wound infection, delayed wound healing, and delayed discharge.
Hyperthermia
Hyperthermia happens less frequently and when it’s malignant it can be fatal. Hyperthermia can cause fever, dilated blood vessels, increased circulation, higher heart rate, pain, and significant medical interventions.
Temperature management complications create problems for patients, healthcare professionals, and hospitals.
Patients can experience severe complications during and after surgery, delay in recovery, and sometimes even death.
OR and PACU clinicians have enough going on already, having to take additional measures to treat hypothermia or hyperthermia creates an additional burden for them and the patient.
Hospitals experience increased costs, delayed patient discharge, and a decrease in patient satisfaction.
Standards and Guidelines
WHO
The World Health Organization (WHO) recommends that body temperature should be measured continuously in patients in whom a change is anticipated, intended, or suspected. This can be done by continuous electronic temperature measurement, if available.4
MHAUS
The Malignant Hyperthermia Association of the United States (MHAUS) recommends core temperature monitoring for all patients given general anesthesia lasting more than 30 minutes.5
ASA
American Society of Anesthesiologists (ASA) recommends that every patient receiving anesthesia shall have temperature monitored when clinically significant changes in body temperature are intended, anticipated, or suspected.2
AST
Association of Surgical Technologists (AST) recommends that measures to monitor and maintain body temperature should begin in the preoperative phase and continue into the postoperative phase of the surgical procedure.6
Our Temperature Management Solution
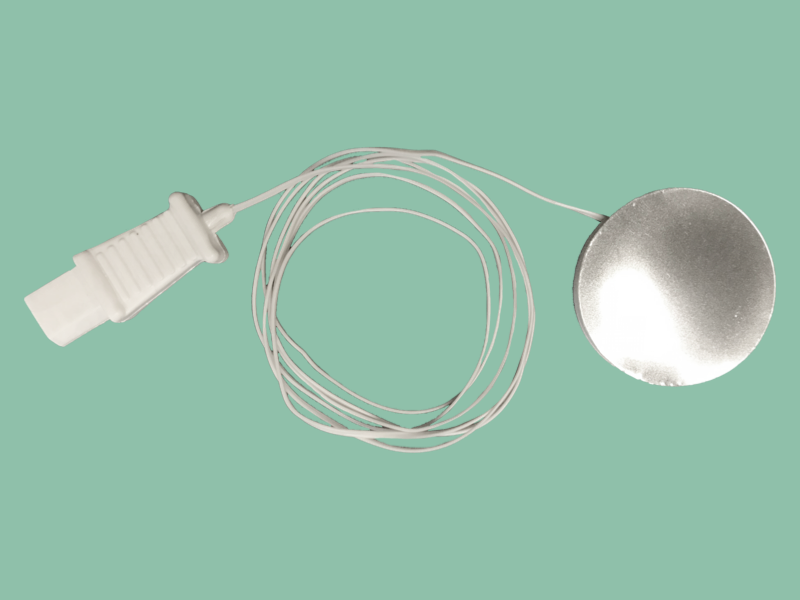
Temperature Cables
Our temperature monitoring products are made with patient care in mind and specifically designed with features that help reduce the risk device-related injury. Remember to monitor and protect every patient, every time with Starboard Medical’s temperature monitoring products.
- Jessica D., Shannon L. and Patricia R. How many in-patient surgeries were performed in the US by year during 2015, 2016, and 2017? December 29, 2017. Wonder. Retrieved from: https://askwonder.com/research/in-patient-surgeries-performed-us-year-during-2015-2016-2017-qmkm6vxov
- American Society of Anesthesiologists. (2010). Standards for Basic Anesthetic Monitoring. Retrieved from https://www.asahq.org/standards-and-guidelines/standards-for-basic-anesthetic-monitoring
- Larach MG, Brandom BW, Allen GC, Gronert GA, Lehman EB. Malignant hyperthermia deaths related to inadequate temperature monitoring, 2007-2012: a report from the North American malignant hyperthermia registry of the malignant hyperthermia association of the United States. Anesth Analg. 2014 Dec;119(6):1359-66. doi: 10.1213/ANE.0000000000000421. PMID: 25268394.
- World Health Organization. (2009). WHO Guidelines for Safe Surgery. Retrieved from https://apps.who.int/iris/bitstream/handle/10665/44185/9789241598552_eng.pdf;jsessionid=C05CABA9C3E70224BE6612F86CA563C1?sequence=1
- Malignant Hyperthermia Association of the United States. (2012). Temperature Monitoring During Surgical Procedures. Retrieved from https://www.mhaus.org/healthcare-professionals/mhaus-recommendations/
- Association of Surgical Technologists. (2019). AST Guidelines for Best Practice in Maintaining Normothermia in the Perioperative Patient. Retrieved from https://www.ast.org/uploadedFiles/Main_Site/Content/About_Us/ASTGuidlinesNormothermia.pdf